Key Takeaways:
- Advancements in dental implant technology are improving the natural feel and function of replacements.
- Maintaining good oral hygiene is crucial for preventing infections and ensuring the longevity of dental implants.
- Preserving natural teeth is often preferable; unnecessary extractions for implants should be avoided.
Introduction
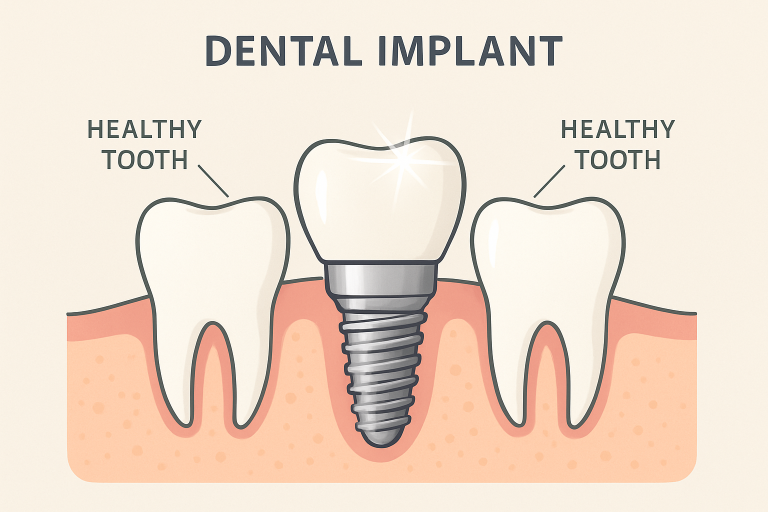
Dental implants have increasingly become the gold standard for replacing missing teeth, offering a highly durable and aesthetically pleasing option that restores both function and appearance to one’s smile. Over the past several decades, dental implants have seen tremendous advancements in both their materials and design, as well as the surgical techniques used for their placement. While the traditional goal was to replace lost teeth, today’s innovations aim to replicate the complexity and unique sensory experience that natural teeth provide. Implants are designed not just to fill in gaps but to fully restore a patient’s bite, comfort, and confidence—with some solutions even reaching the point where they are virtually indistinguishable from natural teeth, much like the comprehensive alignment care provided by an orthodontist chicago.
For those interested in more comprehensive rehabilitation, exploring options for full-mouth dental implants at https://www.ora4x.com/services/dental-implants/full-mouth-dental-implants/ can provide both functional and cosmetic benefits as technology continues to advance. As dental implant procedures become more popular, the focus in academic and clinical dentistry has shifted towards ensuring these solutions not only look great but also feel and perform as closely as possible to one’s original teeth.
With demand on the rise, researchers and clinicians are focusing their efforts on enhancing not only aesthetics but also the true oral sensory experience and long-term oral health outcomes for all patients. This article explores groundbreaking advancements in implant technology, methods to prevent implant-related complications, and the important ethical considerations that guide responsible treatment planning in modern implant dentistry.
Advancements in Implant Technology
“Smart” Dental Implants Improving Sensory Feedback
One longstanding issue with traditional dental implants has been the lack of tactile feedback—real teeth allow you to perceive force, texture, and temperature, while conventional implants do not. Fortunately, breakthroughs are changing this reality. At Tufts University, researchers have developed innovative “smart” dental implants that have the potential to bring back a sense of feeling in implanted teeth. These cutting-edge devices incorporate a specially engineered biodegradable coating that promotes the growth of nerve tissue in the surrounding area of the implant fixture. The goal is for patients to regain much of the sensory feedback that natural teeth provide, allowing them to detect if they’re biting too hard, discern different food textures, and enhance their overall oral awareness.
This leap in technology doesn’t just benefit comfort or satisfaction—it could improve chewing efficiency, allowing individuals with these implants to chew foods of varying textures with greater ease. It could restore subtle speech abilities, such as proper pronunciation of certain sounds, that are sometimes impaired by traditional implants. The significance of such technology is especially notable for patients needing multiple or full-mouth implants, as restoring natural sensation can make a profound difference in quality of life. Furthermore, companies focused on high-tech dental solutions are exploring ways to apply these smart materials more broadly, ensuring that such advancements endure in the complex, bacteria-rich environment of the mouth while remaining safe for long-term use.
Preventing Implant-Related Infections
While the mechanical success of dental implants is impressive, the true measure of a successful outcome lies in maintaining long-term oral health. One of the most significant risks to implant longevity is a condition known as peri-implantitis, an infection and resulting inflammation that develops around the implant, affecting both the surrounding gum tissue and the underlying bone. Peri-implantitis is a major concern because, if left untreated, it can lead to loss of bone support and eventual implant failure. Research has shown that up to 20% of dental implant patients may experience some form of peri-implantitis in their lifetime.
The cornerstone of preventing such infections is meticulous oral hygiene. Patients are advised to practice diligent daily brushing, flossing, and the use of antimicrobial rinses, all tailored to their specific needs as recommended by dental professionals. Regular dental visits for professional cleaning and early detection of potential issues are essential parts of a post-implant care plan. Dentists and hygienists regularly update their education to stay ahead of potential risks presented by new implant systems and materials, making continuing education an essential element of implant aftercare.
Innovative cleaning regimens and the development of new antimicrobial agents are proving successful, significantly reducing the likelihood of bacteria-driven complications. For patients who are more prone to gum disease or have complex dental histories, customized prophylactic plans may be available, which may involve more frequent visits or adjunctive therapies. Staying informed, maintaining good habits, and leveraging modern preventive strategies are crucial steps for anyone with implants.
Ethical Considerations in Implant Dentistry
Preserving Natural Teeth Over Implants
Despite the immense benefits of dental implants, concerns have arisen around the overuse of implant procedures in cases where natural teeth could otherwise be saved. Increasingly, some practitioners and health organizations warn that unnecessary extraction of healthy or salvable teeth—sometimes driven by financial motives rather than best patient outcomes—may compromise long-term oral function and health. The American Academy of Periodontology and similar bodies emphasize that preserving natural teeth should always be the preferred choice, as native teeth possess a unique biology and attachment to the jaw that no artificial substitute can fully replicate. Once a tooth is lost, multiple structures are affected, which can alter bite, jaw stability, and even facial appearance.
Patients seeking implants should always receive a thorough examination, with careful consideration given to all available restorative options. Obtaining a second opinion can be invaluable in complex cases or when a provider recommends extracting teeth that appear otherwise healthy. The best clinicians will present a balanced view of the risks, benefits, and alternatives, empowering patients to make truly informed choices for their long-term health.
Responsible providers consider more than just the clinical or financial aspects; they factor in the individual’s oral health history, current health status, future needs, and, importantly, the patient’s goals and expectations. Transparent communication, ethical practice standards, and prioritizing lasting function and well-being—all are hallmarks of patient-centered dentistry.
Conclusion
Innovations in dental implant technology continue to transform the landscape of restorative dentistry, offering patients hope for improved outcomes, enhanced comfort, and increased long-term satisfaction with their dental care. Keeping up with the latest advances—whether that means smart implants that restore built-in sensory feedback or the development of more effective infection-prevention protocols—benefits both patients and clinicians alike. Ultimately, patients are most likely to succeed when they work with experienced, ethical dental professionals who provide clear communication, seek to preserve what is naturally healthy, and leverage the best available technology to restore both the appearance and function of a natural smile.